The other day, I got an email message from the Academy of Consultation-Liaison Psychiatry (ACLP). It was from the Med-Psych Special Interest Group (SIG). It was an intriguing question about a paper somebody was looking for and having trouble getting it through the usual channels.
The paper was “The Liaison Psychiatrist as Busybody” by somebody named G.B. Murray and published in the Annals of Clinical Psychiatry in 1989. The person looking for the paper mentioned that there was a note from the editor that the paper was of a “controversial nature.”
I was immediately intrigued after doing a search of my own and finding out that the full note from the editor was as follows:
“Editor’s Note: We are aware of the controversial nature of this communication and invite responses from psychiatrists in practice as well in academic settings.”
Nothing is as exciting as holding something out to us and at the same time hiding it from us. Why was it unavailable through the usual channels? Nowadays “usual channels” means accessing the digital copy over the internet from the journal.
Anyway, soon enough somebody found a copy of what turned out to be Dr. George B. Murray’s presentation of the paper with the title “The Liaison Psychiatrist as Busybody” at the American Psychiatric Association (APA) meeting in 1983 in New York. It looked like it was copied from the Annals of Clinical Psychiatry journal where it was published in 1989.
The paper was one of four APA presentations (p. 76) in a symposium entitled “The Myth of Liaison Psychiatry.” The titles and presenters including Murray’s:
- Teaching Liaison Psychiatry as Medicine at Massachusetts General Hospital—Ned Cassem MD, Boston, MA
- The Liaison Psychiatrist as Busybody—George Murray MD, Boston, MA
- Liaison Psychiatry to the Internist—John Fetting, MD, Baltimore, MD
- The Hazards of “Liaison Psychiatry”—Michael G. Wise, MD, Baltimore, MD
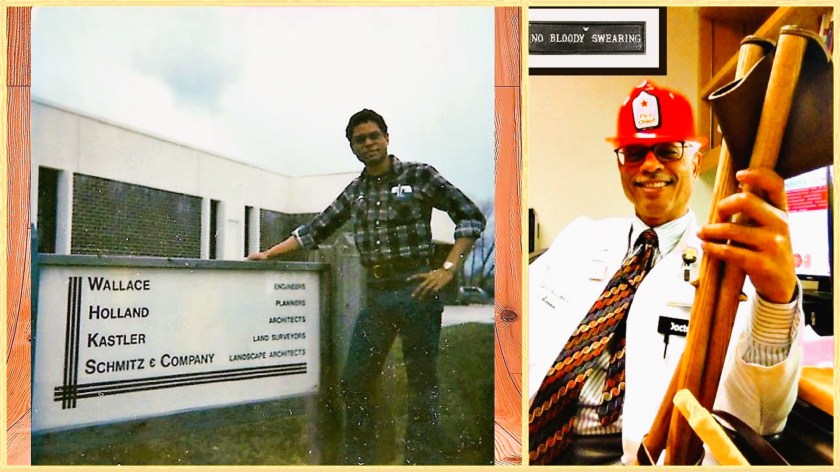
Before I get to the paper itself, I should mention that it was my wife, Sena, who gets the credit for actually finding out that “G.B. Murray” was George B. Murray, a distinguished consultation psychiatrist at Massachusetts General Hospital.
I purposely omitted the word “liaison” from “consultation psychiatry” because he was said to have “loathed the word ‘liaison’.” This was according to the blogger (Fr Jack SJ MD) who posted an in-memoriam piece on his blog in 2013 shortly after Father George Bradshaw Murray died. He had been a Jesuit priest as well as a psychiatrist. Fr Jack SJ MD also noted that Murray ran the consult fellowship at Mass General, saying:
“George’s fellowship was unique. He founded it in 1978 and directed it full-time until a few years ago. By the time he retired he had trained 102 fellows mostly on his own. His didactic methods would be frowned upon by politically-correct, mealy-mouthed, liberals of academe (bold face type by J. Amos). His fellows thrived. George turned us, in the words of Former Fellow Beatriz Currier, MD, “into the kind of psychiatrist I wanted to be but didn’t know how to become.” We worked hard. Many consults per day. Vast amounts of reading for which he expected us to be prepared. But he worked even harder for us.”
So, right about now, to quote one of my favorite Men in Black movies character, Agent J: “That grumpy guy’s story’s starting to come into focus a little bit here.”
I’m not going to dump big quotes from Murray’s presentation, but I can say that it’s understandable to me now why it has been described as controversial. He just sounds a little testy.
Getting back to the New York symposium, I noticed that the chairperson was Thomas P. Hackett, and the co-chair was Ned Cassem, both of Mass General, the latter also a Jesuit priest. I never met either of them, but they are legends. Hackett died in 1988 and Cassem died in 2015.
I’ve read what Hackett wrote about the difference between psychiatric consultation and psychiatric liaison:
“A distinction must be made between a consultation service and a consultation liaison service. A consultation service is a rescue squad. It responds to requests from other services for help with the diagnosis, treatment, or disposition of perplexing patients. At worst, consultation work is nothing more than a brief foray into the territory of another service, usually ending with a note written in the chart outlining a plan of action. The actual intervention is left to the consultee. Like a volunteer firefighter, a consultant puts out the blaze and then returns home. Like a volunteer fire brigade, a consultation service seldom has the time or manpower to set up fire prevention programs or to educate the citizenry about fireproofing. A consultation service is the most common type of psychiatric-medical interface found in departments of psychiatry around the United States today.
A liaison service requires manpower, money, and motivation. Sufficient personnel are necessary to allow the psychiatric consultant time to perform services other than simply interviewing troublesome patients in the area assigned. He must be able to attend rounds, discuss patients individually with house officers, and hold teaching sessions for nurses. Liaison work is further distinguished from consultation activity in that patients are seen at the discretion of the psychiatric consultant as well as the referring physician. Because the consultant attends social service rounds with the house officers, he is able to spot potential psychiatric problems.”—T. P. Hackett, MD.
Here’s the thing. This quote comes from Hackett’s chapter in the 1978 edition of the Massachusetts General Handbook of General Hospital Psychiatry. But I tended to gloss over what he wrote right below it:
“Once organized, a liaison service tends to expand. Most liaison services are appreciated and their contribution is recognized. Sometimes this brings tangible benefits such as space and salary from the departments being serviced. However, even under the best circumstances, the impact of a liaison effort seldom lingers after the effort is withdrawn. Lessons taught by the psychiatrist need constant reinforcement or they are forgotten by our medical colleagues. In a way, this is an advantage since it ensures a continuing need for our presence. Conversely, it disappoints the more pedagogical, because their students, while interested, fail to learn. I believe we must be philosophical. After all, our surgical colleagues do not insist that we learn to do laparotomies. They insist only that we be aware of the indications.”—T.P. Hackett, MD.
You get a clear sense of Hackett’s sense of humor as well as a practical appreciation of what can and maybe cannot be done when you try to apply liaison principles in a formal teaching approach.
So, what does Murray say about liaison psychiatry that seemed cloaked behind the term “controversial”? He starts off by admitting that his remarks will be “inflammatory” and makes no apology for it. He starts with three main statements:
- What all nonpsychiatric physicians appreciate, and what, in fact, works, is the medical model of consultation psychiatry.
- Liaison psychiatry is more myth than reality.
- The liaison psychiatrist is to a great extent a relatively high-status busybody.
It’s difficult to pick out excerpts from Murray’s presentation—so much of it is integral to the main message and entertaining as well that I hate to omit it. Here’s my pick anyway:
“There is a certain Olympian quality surrounding liaison psychiatrists. It is as if they will teach others the wonders of the labyrinthine biopsychosocial factors involved in patient care. The other Olympian feature centers on the so-called consultee-oriented consultation. In hearing discussions and reading the literature one can get a downwind whiff of antiphysician feeling. There are remarks made, for example, of the insensitivity of surgeons, of patient “harassment” and how little the attending physician understands this hysteric’s or sociopath’s inner dynamics. This attitude is snobbish, unhelpful, and in semistreet parlance, “chickendip.” It does not seem to bother liaison psychiatrists that there are no liaison cardiologists, liaison endocrinologists, and so forth—another clue to the vacuity of liaison psychiatry.”
He is testy and with good reason, if you define liaison in this way. His paper is uproarious. And there are lots of controversies in medicine. I’m still not sure why this one seemed hidden from public view.
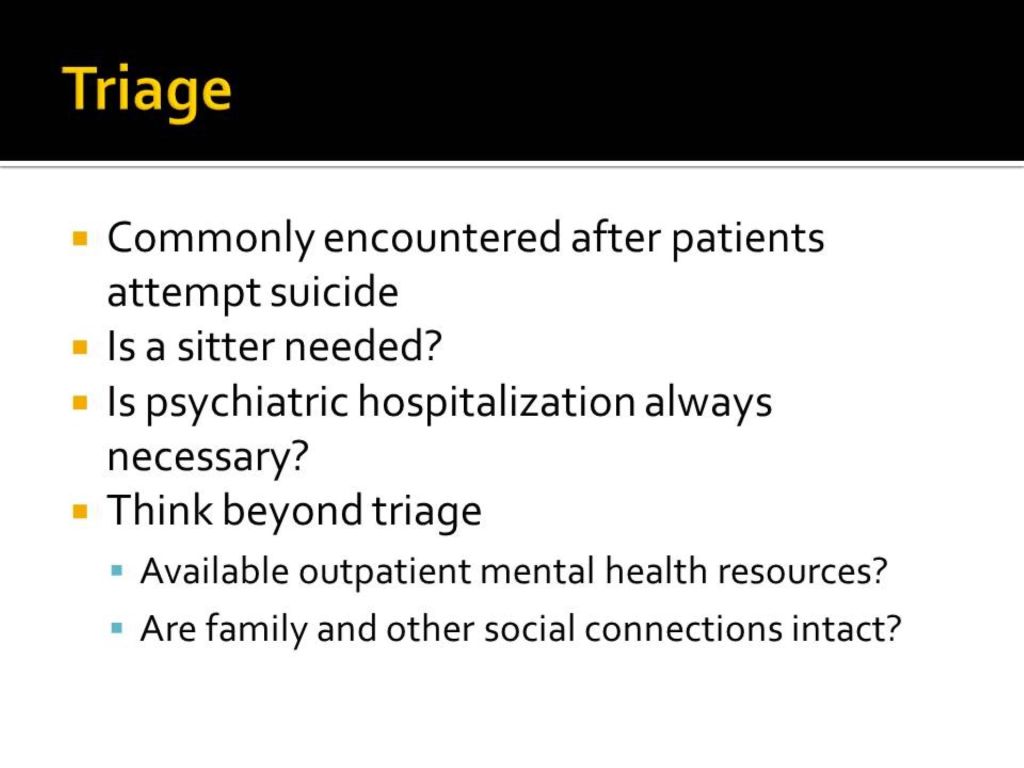
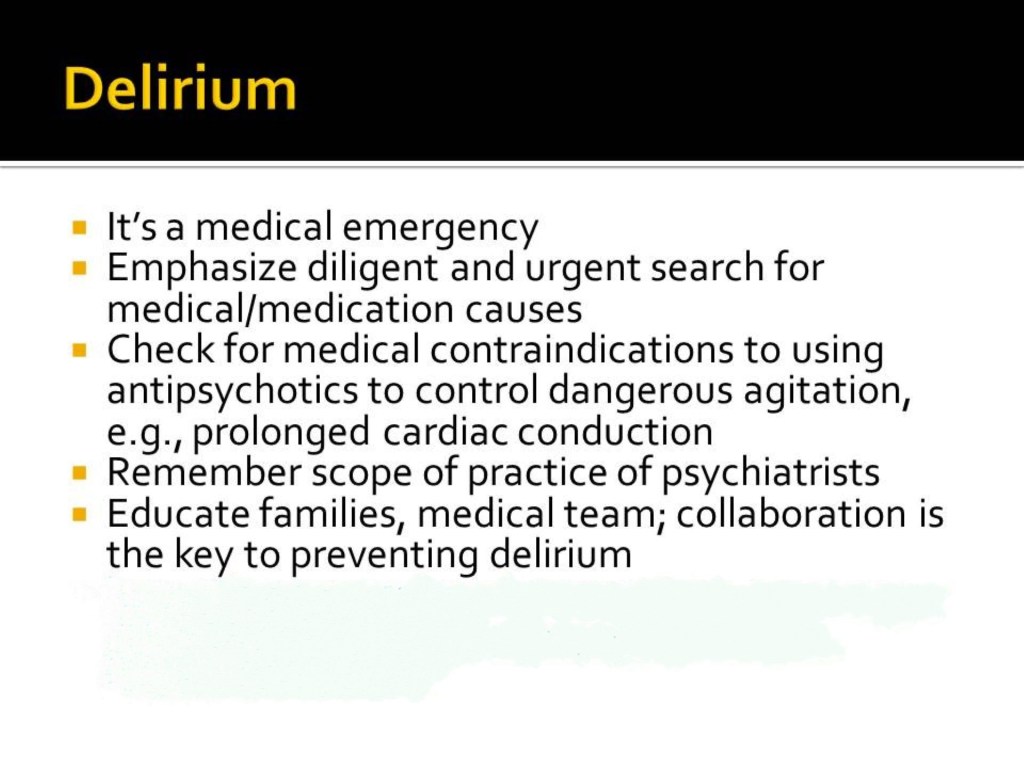
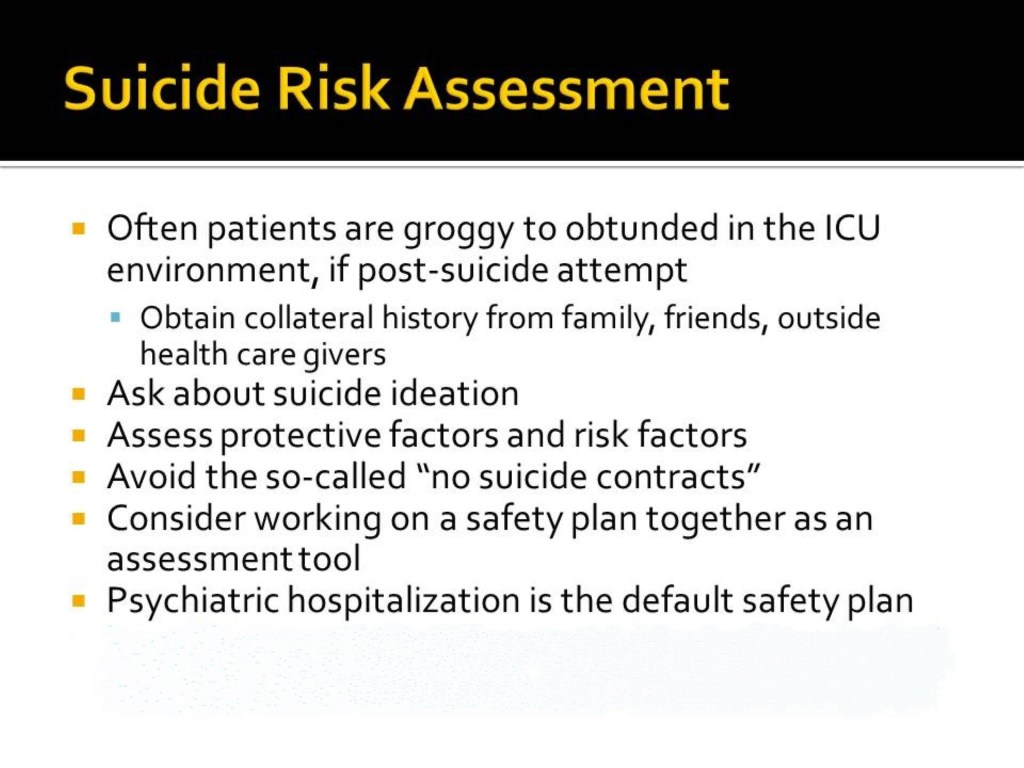
I opened up the door by saying “…if you define liaison in this way.” There are other ways to convey useful information to “consultees.” For example, I had better luck talking in a casual way about what I could for a MICU medicine resident about how to help manage a very agitated delirious patient on a ventilator who was in restraints because of the fear of self-extubation (a common problem psychiatric consultants get called about).
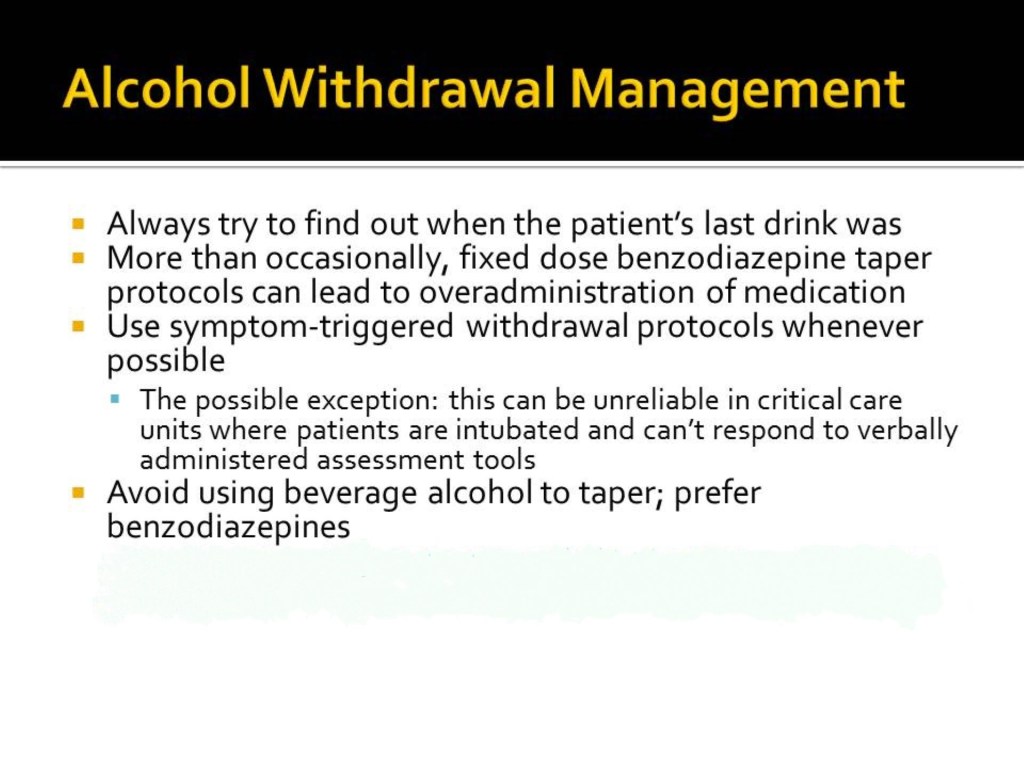
We were sitting in the unit conference room and the unit pharmacist was present. I don’t remember if the attending was there. I started to describe what had been studied in the past, which was continuous intravenous infusions of haloperidol lactate (there are several studies which do not support the use of haloperidol for treating delirium). There was no way to administer oral sedatives. In fact, the patient was being given heavy doses of intravenous benzodiazepines and opioids.
I notice that the more details I shared about the intravenous haloperidol, the wider the pharmacist’s eyes got. Long story short, the MICU resident decided to try something other than psychiatric medication. Indirectly, you could say I was using a motivational interviewing technique to teach. But Murray would have described that as Olympian and in any case, I didn’t consciously do that. All I had were facts and I told the resident what they were. A matter-of-fact approach and tact can be part of a liaison approach, but that’s not what Murray was concerned about and probably not what he saw from most liaison psychiatrists.
And I had to work hard not to display testiness (much less loftiness), which I’m afraid I didn’t always do.