Below is an old post from a previous blog that I published on June 6, 2010. Although the title in my record is simply PM Handbook Blog, there must have been another title. Maybe it should have been more like The Chicken Has Finally Laid an Egg (you’ll get the joke later).
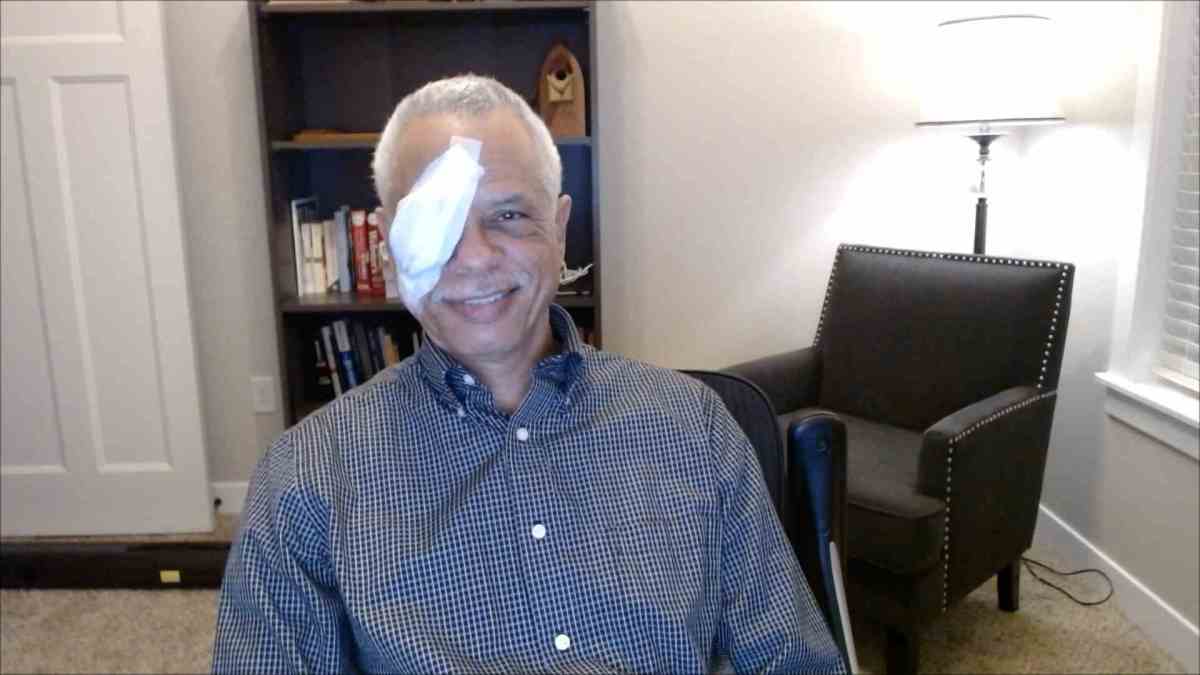
There are two reasons for posting it today. One is to illustrate how the Windows voice recognition dictation app works. It’s a little better than I thought it would be. The last time I used it, it was ugly. I’m using it now because I thought it might be a little easier than trying to type it since I still have problems with vision in my right eye because of the recent retinal tear injury repair. So, instead of doing copy paste, what you’re seeing is a dictation—for the most part.
On the other hand, I’m still having to proofread what I dictate. And I still find a few mistakes, though much fewer than I expected.
The other reason for this post is to help me reflect on how far the fellowship has come since that time. It did eventually attract the first fellow under a different leader. That was shortly after I retired. It was a great step forward for the department of psychiatry:
“Here is one definition of a classic:
“Classic: A book which people praise but don’t read.” Mark Twain.
When I announced the publishing of our book, Psychosomatic Medicine, An Introduction to Consultation Liaison Psychiatry, someone said that it’s good to finally get a book into print and out of one’s head. The book in earlier years found other ways out of my head, mainly in stapled, paperclipped, spiral bound, dog eared, pages of homemade manuals, for use on our consultation service.

It’s a handbook and meant to be read, of course, but quickly and on the run. As I’ve said in a previous blog, it makes no pretension to being the Tour de Force textbook in America that inspired it. However, any textbook can evolve into an example of Twain’s definition of a classic. The handbook writer is a faithful and humble steward who can keep the spirit of the classic lively.
We must have a textbook as a marker of Psychosomatic Medicine’s place in medicine as a subspecialty. It’s like a Bible, meant to be read reverently, venerated, and quoted by scholars. But the ark of this covenant tends to be a dusty bookshelf that bows under the tome’s weight. A handbook is like the Sunday School lesson plan for spreading the scholar’s wisdom in the big book.
Over the long haul, the goal of any books should mean something other than royalties or an iconic place in history. No preacher ever read a sermon to our congregation straight out of the Bible. It was long ago observed by George Henry that there will never be enough psychiatric consultants. This prompts the question of who will come after me to do this work. My former legacy was to be the Director of a Psychosomatic Medicine Fellowship in an academic department in the not-so-distant past. Ironically, though there will never be enough psychiatric consultants, there were evidently too many fellowships from which to choose. I had to let the fellowship go. My legacy then became this book, not just for Psychosomatic Medicine fellows, but medical students, residents, and maybe even for those who see most of the patients suffering from mental illness—dedicated primary care physicians.
My wife gave me a birthday card once which read: “Getting older: May each year be a feather on the glorious Chicken of Life as it Soars UNTAMED and BEAUTIFUL towards the golden sun.” My gifts included among the obligatory neckties, a couple of books on preparing for retirement.

Before I retire, I would like to do all I can to ensure that the next generation of doctors learn to respect the importance of care for both body and mind of each and every one of their patients. That’s the goal of our book. And may the glorious chicken of life lay a golden egg within its pages to protect it from becoming a classic.”
Chicken picture credit: Pixydotorg.