So, I have to hurry up and get these 3 photos posted for today because it’s getting pretty late. Recall the Iowa Healthiest State Initiative calendar along with my photos to share:
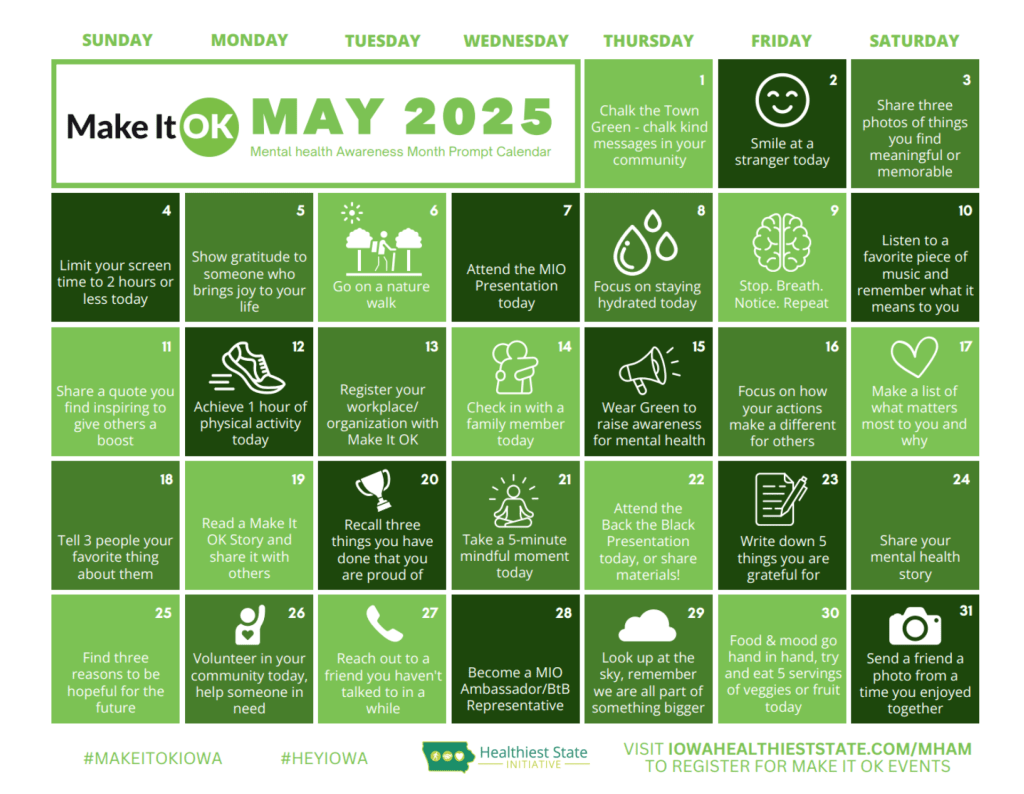


The images are important features of events in my life or my sense of humor.
I’m a birdwatcher and many different species of birds visited the fountain. The fountain attracted bluebirds who splashed and even swam in it. That fountain was very heavy. We couldn’t leave it out all winter. In the fall I had to lift the bowls off and move them somewhere else. Moving them entailed lifting them onto bags of mulch so as to reduce the work of hefting them a small distance at a time. The birds were beautiful to watch.
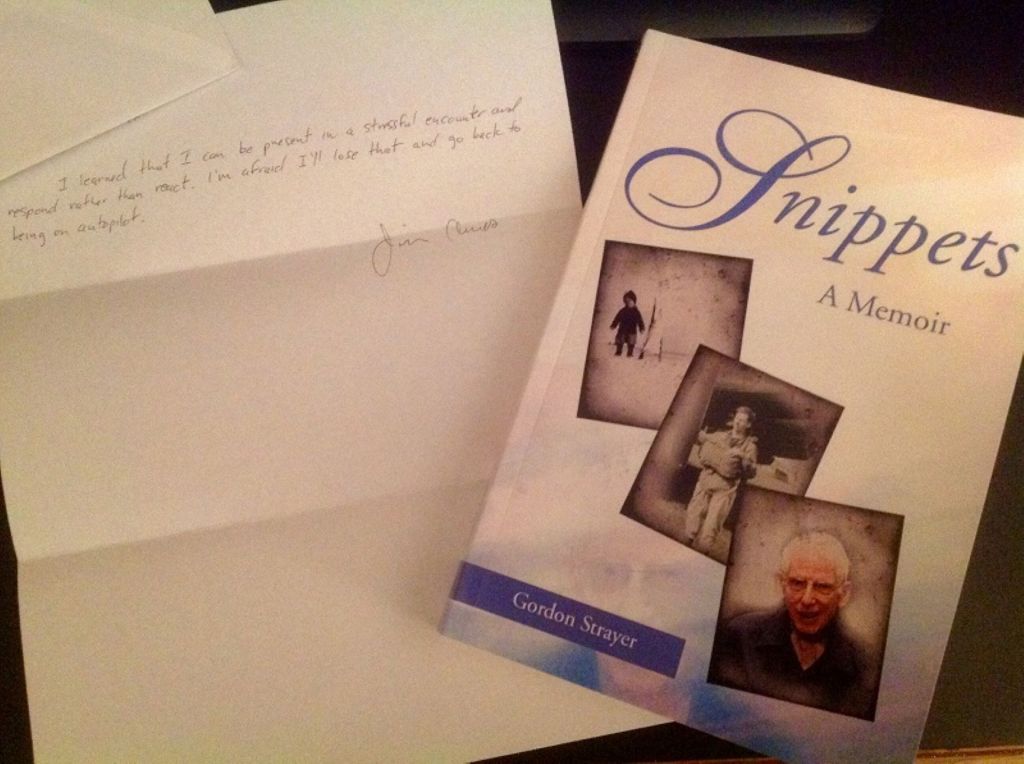
The letter was a class assignment our Mindfulness Based Stress Reduction (MBSR) teacher had us write at the beginning of the class. After we graduated, she mailed us those letters shortly thereafter. We were to write something connected with what we thought we had gained or what we thought might happen after taking the MBSR class. The book might seem out of place, and while I can’t talk much about Gordon Strayer, I did meet him and read his book (which is now long gone; probably lost in a move). I admired him. I don’t think he feared death.
The Chrysler Building reminds me of the Men in Black (MIB) 3 movie, and I included it because my sense of humor is very important to me. In the movie, Agent J and Jeffrey Price have this funny conversation about time travel back to an era that was not the greatest for black people. I know because I lived through it. Agent J is about to use the time travel device which involves jumping off a tall building (it’s a “time jump!”). Agent J is preparing to travel back in time to M.I.B.’s early days in 1969 to stop an alien from assassinating his friend Agent K and changing history. They have this short conversation:
Jeffrey Price: Do not lose that time device or you will be stuck in 1969! It wasn’t the best time for your people. I’m just saying. It’s like a lot cooler now.
Agent J: How will I know if it works?
Jeffrey Price: You’ll either know…or you won’t.








