I want to gas; I mean talk about copyright as it relates to consultation psychiatry or telling dad jokes. By the way, those aren’t the same.
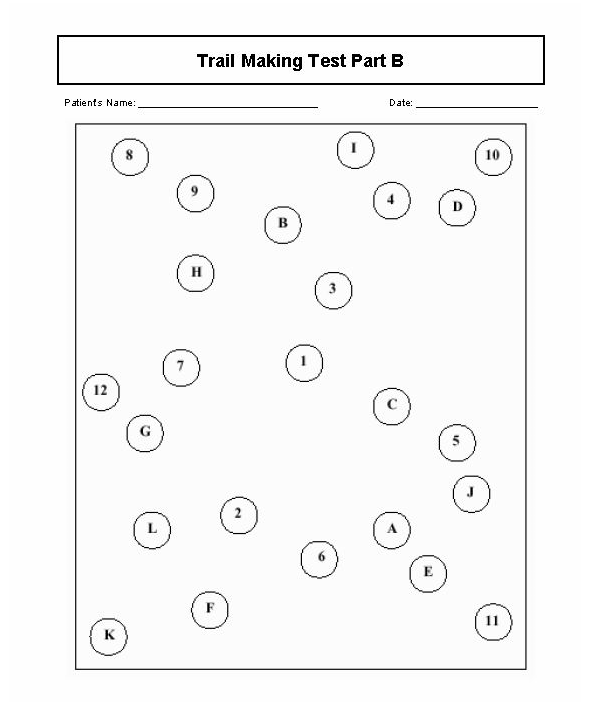
I used to teach medical students and residents how to do certain quick bedside cognitive tests for delirium and dementia. Over the years the instructions about how to administer them (and the restrictions over using them at all) have changed slightly. The major point to make is that they have been copyrighted, which usually means you have to pay to play.
One of them, the Mini Cog, despite being copyrighted, does not require you to pay for the privilege of using it. The video below shows part of it. I didn’t do a comedy bit about the short term recall of 3 objects. The video also flickers when I show the delirium order set; just pause it to stop the flickering.
There used to be a cognitive assessment called the Sweet 16, which started off being non-copyrighted, but then became copyrighted. At first the Sweet 16 mysteriously just disappeared from the internet. You can now download it from the internet, but it’s clearly marked as copyrighted.
The reason the Sweet 16 became unavailable is because a company called Psychological Assessments Resource (PAR) acquired the copyright and then started enforcing it. I found out about this when I could not obtain the PAR version of a cognitive assessment very similar to the Sweet 16 called the Mini Mental State Exam (MMSE) unless I forked over at least $100.
I then started teaching trainees how to use the Montreal Cognitive Assessment (MoCA) because it was free to use without any strings attached. Then it also was copyrighted although you can use it under certain conditions.
Moving right along to telling dad jokes, I found out that dad jokes (and indeed, any joke) can be copyrighted, at least in theory. In fact, it’s hard to enforce the copyright on jokes, even when you can prove originality. Here’s an example of a dad joke I think I made up:
What do you get when you cross marijuana with a Mexican jumping bean? A grasshopper.
Note: this joke may become more important now that the DEA, according to news agencies, plans to reclassify marijuana from Schedule I to III in the near future.
Sena thought it was funny (the joke, not the DEA), which probably means it’s not, technically, a dad joke. That’s according to the authority about dad jokes, Dad-joke University of Humour, (DUH). I’m far from a joke teller at all, as Sena (and anyone else who knows me) would assert. On the other hand, I did graduate from DUH and have a diploma to prove it. You can now give me money.

Furthermore, I also investigated whether something called anti-jokes can be copyrighted. According to the internet, the answer seems to be no. Here’s my attempt of the anti-joke:
Knock, knock.
Who’s there?
The doorbell salesman.
See what I did there? In case you didn’t know, experts say that Knock-Knock jokes are among the hardest to copyright for reasons I suggest you look up later. If you also frame the Knock-Knock joke as an anti-joke (stay with me here), the literalness and mundanity of the so-called punch line makes it virtually impossible to copyright. And, like the dad joke, it’s usually not funny—although there can be exceptions.
Just for the sake of incompleteness, I’ll mention the concept of copyleft, which is not the same as open-source. Although this is usually applicable to computer software, you could broaden it to include dad jokes—I think. Copyleft could mean you can use or modify a dad joke (or anti-joke), spread it freely at parties and whatnot as long as it’s bound by some condition. This includes paying me (no personal checks, please).
What pet do inventors have a love-hate relationship with? A copycat.
You’re welcome.