I just saw the Clinical Psychiatry News article “Evidence poor on medical marijuana for neuropathic pain,” by Andrew D. Bowen. It was published May 2019, Vol. 47, No. 5 and I couldn’t find it on line yet.
I should also hasten to add that there are a couple of other important articles on management of pain in this issue of Clinical Psychiatry News. One of them expresses a similar opinion about the lack of clear evidence pointing to a clear best choice for a medication for neuropathic pain, “No clear winner emerges for treating for chronic pain” also by Andrew D. Bosen, who interviewed a neurologist, Dr. Raymond Price, associate professor of neurology at the University of Pennsylvania, Philadelphia about his review of the evidence for treatment of neuropathic pain.
In addition, on a more hopeful note, there is good evidence for the effectiveness of cognitive behavioral therapy (CBT) for chronic pain, “In chronic pain, catastrophizing tied to disrupted circuitry,” by Kari Oakes, who interviewed Drs. Robert R. Edwards, PhD, psychologist at Brigham and Women’s Hospital/Harvard Medical School (Boston) Pain Management Center, and Vitaly Napadow, PhD. Connectivity between certain areas of the brain can lead to the perception that pain is a part of who we are. This can even interfere with the effectiveness of pain medications.
Dr. Ellie Grossman, MD, MPH said at the annual meeting of
the American College of Physicians that there’s “a lot of the Wild West” in
medical marijuana research regarding its use in neuropathic pain. I got the
impression she was being as diplomatic as she could when she described the level
of evidence as being marked by a lot of “squishiness.”
It’s a frankly cautious comment compared with the more
positive opinions expressed just a month ago in Clinical Psychiatry News. Dr.
Grossman is quoted, “The upshot here is that there may be some evidence for
neuropathic pain, but the evidence is generally of poor quality and kind of
mixed.” Dr. Grossman is an instructor at Harvard Medical School and Primary Care
Lead for Behavior Health Integration, Cambridge Health Alliance, Somerville,
Massachusetts.
In fact, as the author points out, the research in this area
is marked by inconsistencies in the medical marijuana formulations, small
numbers of patients enrolled in studies, and equivocal results from
meta-analyses.
The title of the article says it all and it’s really no surprise.
I have little to add except the following very short opinion based on a very
superficial scan of PubMed.
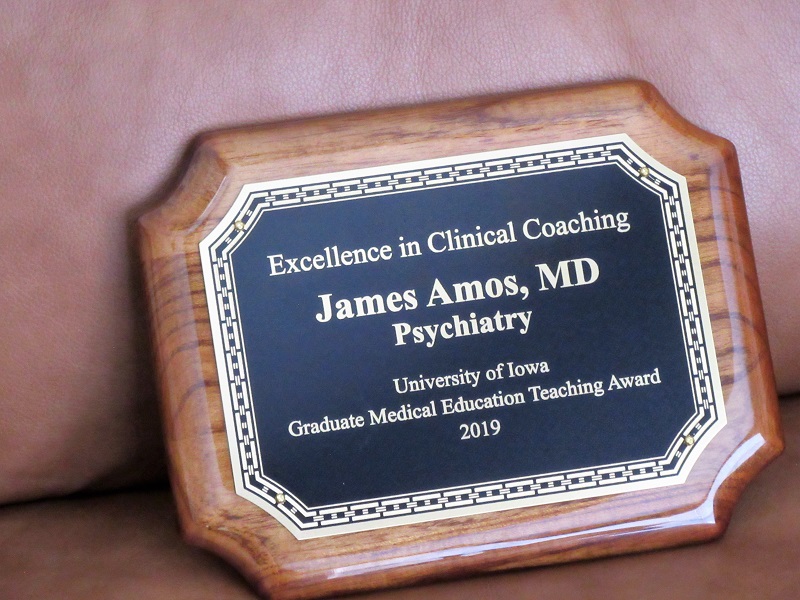
First, I happened to find a couple of papers from the mid-1970s about cannabis and pain in cancer patients. They were written by Russell Noyes, MD and Art Canter, Ph.D. and colleagues. Dr. Noyes has retired for the second time from the Psychiatry Dept at University of Iowa and Dr. Canter was enjoying his retirement until his death in October, 2018; he was in his late 90s.
Even in 1975, there was very little reason for enthusiasm
about the analgesic effect of cannabis in cancer patients. Admittedly, the
number of subjects were low in each study but the side effects of cannabis were
severe in a few cases.
The summary from the first Noyes et al paper is essentially
that, why analgesic effect was demonstrable at high dose levels, so was
“…substantial sedation and mental clouding…”
In the second paper by Noyes et al, the concluding remarks
are telling— “Finally, particular difficulty was experienced in evaluating the
pain of patients after receiving THC. In many instances they appeared
exceptionally peaceful while, at the same time, reporting little pain relief. In
other instances, they claimed that, though the pain was unchanged, it bothered
them less.”
There seems to be nothing new under the sun in this setting
although most of the studies involved patient with chronic non-cancer pain. One
study found some benefit and modest tolerability—see the caveat below (Ware et
al 2015).
“In conclusion, this study suggests that the AEs of medical
cannabis are modest and comparable quantitatively and qualitatively with
prescription cannabinoids. The results suggest that cannabis at average doses
of 2.5 g/d in current cannabis users may be safe as part of a carefully
monitored pain management program when conventional treatments have been
considered medically inappropriate or inadequate. However, safety concerns in
naive users cannot be addressed. Moreover, long-term effects on pulmonary
functions and neurocognitive functions beyond 1 year cannot be determined.
Further studies with systematic follow-up are required to characterize safety
issues among new cannabis users and should be extended to allow estimation of
longer-term risks.”
See the abstracts below. They tend to echo Dr. Grossman’s
impressions. I wonder whether the quality of the research in this area will
ever be strengthened.
References:
NOYES, R., et al.
(1975). “Analgesic Effect of Delta‐9‐Tetrahydrocannabinol.” The
Journal of Clinical Pharmacology 15(2‐3): 139-143.
Noyes, R., et al.
(1975). “The analgesic properties of delta‐9‐tetrahydrocannabinol and
codeine.” Clinical Pharmacology & Therapeutics 18(1): 84-89.
The administration of single oral doses of delta‐9‐tetrahydrocannabinol
(THC) to patients with cancer pain demonstrated a mild analgesic effect. At a
dose of 20 mg, however, THC induced side effects that would prohibit its
therapeutic use including somnolence, dizziness, ataxia, and blurred vision.
Alarming adverse reactions were also observed at this dose. THC, 10 mg, was
well tolerated and, despite its sedative effect, may have analgesic potential.
Ware, M. A., et al.
(2015). “Cannabis for the Management of Pain: Assessment of Safety Study
(COMPASS).” The Journal of Pain 16(12): 1233-1242.
Cannabis is widely used as a self-management strategy by
patients with a wide range of symptoms and diseases including chronic
non-cancer pain. The safety of cannabis use for medical purposes has not been
systematically evaluated. We conducted a prospective cohort study to describe
safety issues among individuals with chronic non-cancer pain. A standardized
herbal cannabis product (12.5% tetrahydrocannabinol) was dispensed to eligible
individuals for a 1-year period; controls were individuals with chronic pain
from the same clinics who were not cannabis users. The primary outcome
consisted of serious adverse events and non-serious adverse events. Secondary
safety outcomes included pulmonary and neurocognitive function and standard
hematology, biochemistry, renal, liver, and endocrine function. Secondary
efficacy parameters included pain and other symptoms, mood, and quality of
life. Two hundred and fifteen individuals with chronic pain were recruited to
the cannabis group (141 current users and 58 ex-users) and 216 controls
(chronic pain but no current cannabis use) from 7 clinics across Canada. The
median daily cannabis dose was 2.5 g/d. There was no difference in risk of
serious adverse events (adjusted incidence rate ratio = 1.08, 95%
confidence interval = .57–2.04) between groups. Medical cannabis
users were at increased risk of non-serious adverse events (adjusted incidence
rate ratio = 1.73, 95% confidence interval = 1.41–2.13);
most were mild to moderate. There were no differences in secondary safety
assessments. Quality-controlled herbal cannabis, when used by patients with
experience of cannabis use as part of a monitored treatment program over 1
year, appears to have a reasonable safety profile. Longer-term monitoring for
functional outcomes is needed. Study registration The study was registered with
http://www.controlled-trials.com (ISRCTN19449752). Perspective This study evaluated
the safety of cannabis use by patients with chronic pain over 1 year. The study
found that there was a higher rate of adverse events among cannabis users
compared with controls but not for serious adverse events at an average dose of
2.5 g herbal cannabis per day.
Andreae, M. H., et al.
(2015). “Inhaled Cannabis for Chronic Neuropathic Pain: A Meta-analysis
of Individual Patient Data.” The Journal of Pain 16(12): 1221-1232.
Chronic neuropathic pain, the most frequent condition
affecting the peripheral nervous system, remains underdiagnosed and difficult
to treat. Inhaled cannabis may alleviate chronic neuropathic pain. Our
objective was to synthesize the evidence on the use of inhaled cannabis for
chronic neuropathic pain. We performed a systematic review and a meta-analysis
of individual patient data. We registered our protocol with PROSPERO
CRD42011001182. We searched in Cochrane Central, PubMed, EMBASE, and AMED. We
considered all randomized controlled trials investigating chronic painful
neuropathy and comparing inhaled cannabis with placebo. We pooled treatment
effects following a hierarchical random-effects Bayesian responder model for
the population-averaged subject-specific effect. Our evidence synthesis of
individual patient data from 178 participants with 405 observed responses in 5
randomized controlled trials following patients for days to weeks provides
evidence that inhaled cannabis results in short-term reductions in chronic
neuropathic pain for 1 in every 5 to 6 patients treated (number needed to treat
= 5.6 with a Bayesian 95% credible interval ranging between 3.4 and 14). Our
inferences were insensitive to model assumptions, priors, and parameter
choices. We caution that the small number of studies and participants, the
short follow-up, shortcomings in allocation concealment, and considerable
attrition limit the conclusions that can be drawn from the review. The Bayes
factor is 332, corresponding to a posterior probability of effect of 99.7%.
Perspective This novel Bayesian meta-analysis of individual patient data from 5
randomized trials suggests that inhaled cannabis may provide short-term relief
for 1 in 5 to 6 patients with neuropathic pain. Pragmatic trials are needed to
evaluate the long-term benefits and risks of this treatment.
Ashrafioun, L., et al.
(2015). “Characteristics of substance use disorder treatment patients
using medical cannabis for pain.” Addictive Behaviors 42: 185-188.
Background This study was designed to assess the
prevalence and correlates of self-reported medical cannabis use for pain in a
substance use disorder (SUD) treatment program. Method Participants (n=433)
aged 18years and older were recruited from February 2012 to July 2014 at a
large residential SUD treatment program. They completed a battery of questionnaires
to assess demographics, usual pain level in the past three months (using the
11-point Numeric Rating Scale for pain), depression (using the Beck Depression
Inventory), previous types of pain treatments, and lifetime and past-year use
of substances (using the Addiction Severity Index). Using both adjusted and
unadjusted logistic regression models, we compared those who reported medical
cannabis use for pain with those who did not report it. Results Overall, 15% of
the sample (n=63) reported using medical cannabis for pain in the past year.
After adjusting for age, medical cannabis use for pain was significantly
associated with past-year use of alcohol, cocaine, heroin, other opioids, and
sedatives, but was not associated with usual pain level or depression. It was
also associated with past year treatment of pain using prescription pain
relievers without prescriptions. Conclusions These results indicate that
medical cannabis use for pain is relatively common and is associated with more
extensive substance use among SUD patients. Future work is needed to develop
and evaluate strategies to assess and treat individuals who report medical
cannabis for pain in SUD treatment settings.
Hefner, K., et al.
(2015). “Concomitant cannabis abuse/dependence in patients treated with
opioids for non‐cancer pain.” The American Journal on Addictions 24(6):
538-545.
Background and Objectives Cannabis use is common among
patients taking prescription opioids, although rates of concomitant cannabis
use disorder (CUD) have been largely unexamined. CUD may increase safety risks
in those taking opioid pain medications but it is unknown whether cannabis and
opioids function as substitutes (cannabis use is associated with less
prescription opioid use), or rather as complements (cannabis is associated with
increased use of prescription opioids). Methods We examined rates of CUD in a
national sample of Veterans Health Administration (VHA) patients
(n = 1,316,464) with non‐cancer pain diagnoses receiving
opioid medications in fiscal year 2012. Using bivariate analysis to identify
potentially confounding variables associated with CUD (eg, psychotropic
medication, other substance use disorders) in this population, we then utilized
logistic regression to examine rates of cannabis use disorder among individuals
receiving different numbers of opioid prescriptions (0, 1–2, 3–10, 11–19, 20+).
Results Descriptive analysis, largely confirmed by logistic regression,
demonstrated that greater numbers of prescription opioid fills were associated
with greater likelihood of CUD. This relationship was reduced somewhat for
those receiving the most opioid prescriptions (20+) in the logistic regression,
which controlled for potentially confounding variables. Discussion and
Conclusions These results warrant increased attention to CUDs among patients
receiving numerous opioid prescriptions. Increasing legalization of cannabis is
likely to further increase use and abuse of cannabis in patients prescribed
opioids. Scientific Significance These findings suggest that clinicians should
be alert to concomitant CUD and prescription opioid use, as these substances
appear to complement each other. (Am J Addict 2015;24:538–545)