I was thinking about the Clinical Problems in Consultation Psychiatry (CPCP) learning sessions which was introduced to me by one of my first teachers in the University of Iowa Dept of Psychiatry, Dr. William R. (Bill) Yates.
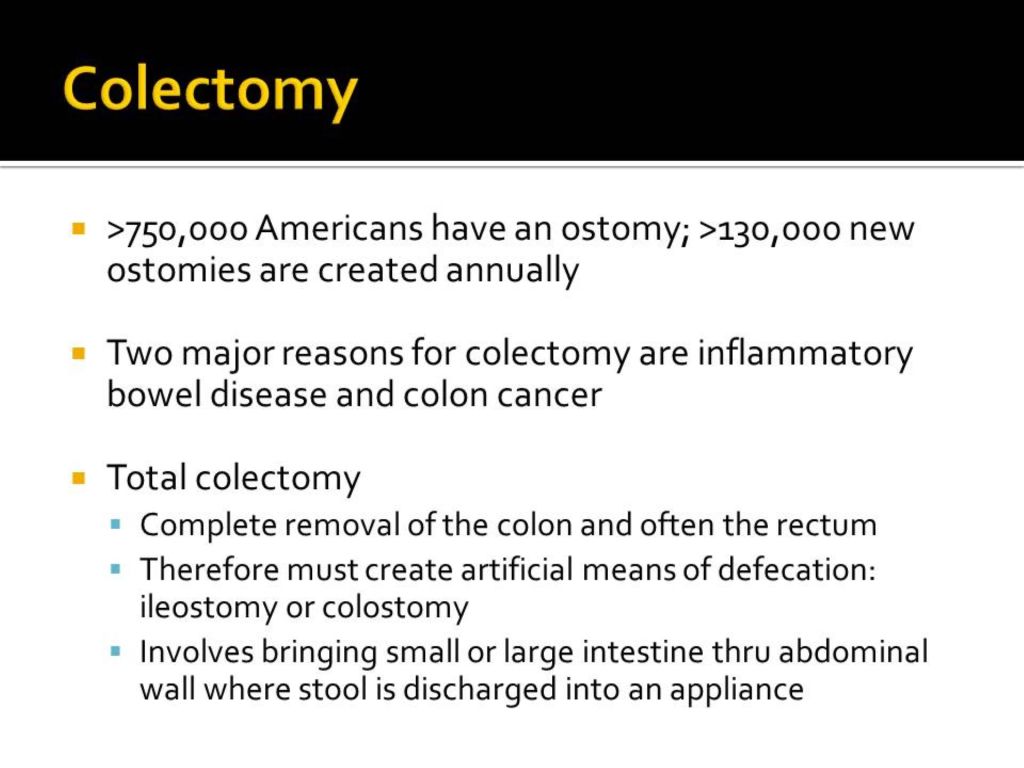
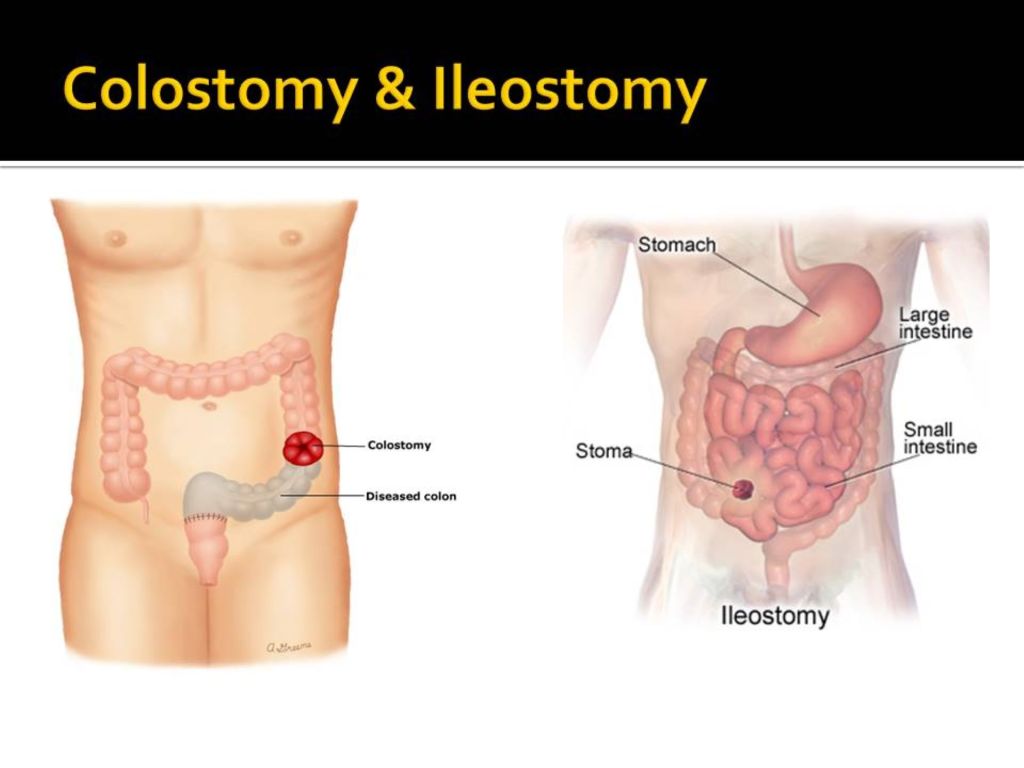
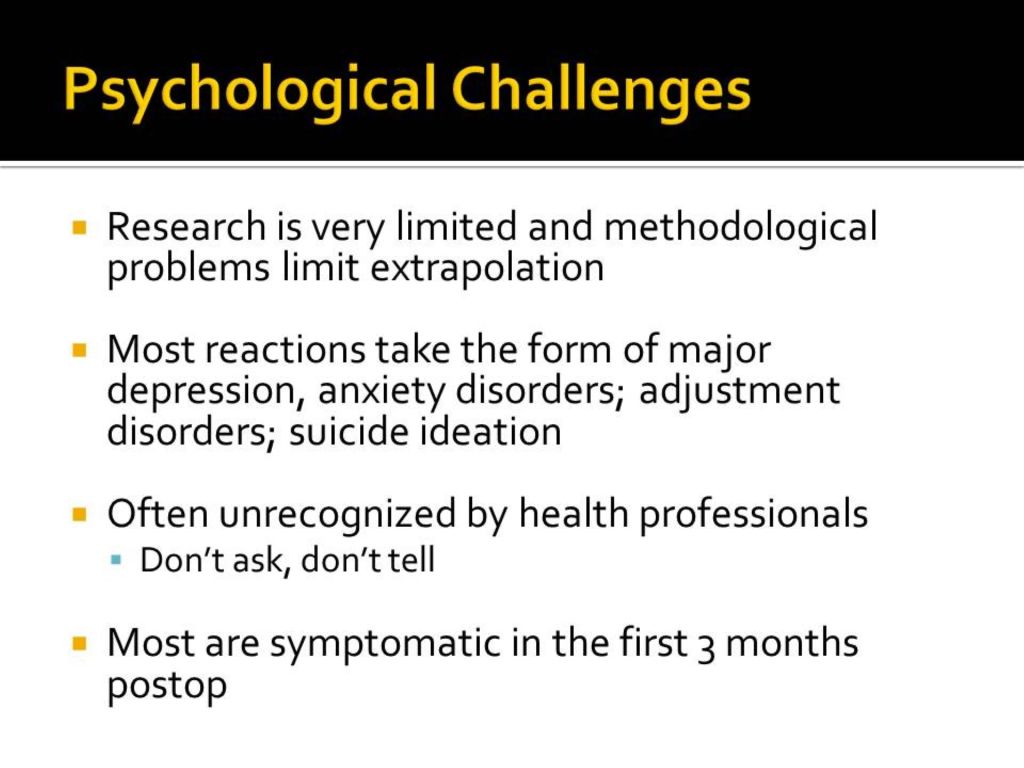
I had originally been thinking of posting one of my own CPCPs that I presented in 2015. It was about the psychosocial adjustment of patients to ostomy.
I searched widely and in vain on the web for any recent information about what Dr. Yates was doing now. I was surprised and saddened to discover his obituary. He died on January 19, 2023 in Tulsa, Oklahoma.
As the obituary says:
He served on the faculty at the University of Iowa for Psychiatry and Family Medicine before becoming Professor and Chair of Psychiatry at the University of Oklahoma College of Medicine in Tulsa. After retiring, he continued to dedicate his time as a volunteer research psychiatrist at OU and the Laureate Institute for Brain Research where he also served on the board of directors. He authored over 100 scientific manuscripts that were published in peer-reviewed journals.
He was an energetic, a great teacher, had a great sense of humor, and was easy to get along with. He published in many scientific journals and taught many trainees. He was an avid bird watcher and his blog Brain Posts highlighting neuroscience research findings is still visible on the web.
He published the paper along with a chief resident on problem-based learning used on the psychiatry consult-liaison service in 1996, the year I graduated psychiatry residency and joined the faculty at The University of Iowa Hospitals & Clinics (Yates, W. R. and T. T. Gerdes (1996). “Problem-based learning in consultation psychiatry.” Gen Hosp Psychiatry 18(3): 139-144.) You can read the abstract for it along with a description of the CPCP at the link above which takes you to my April 19, 2019 blog post “Clinical Problems in Consultation Psychiatry.”
When he was the leader of the psychiatry consult service, we were still using paper charts and his staffing comments were always very brief and encapsulated the assessment and plan succinctly without wasted verbiage—contrasting with my long-winded note.
His remarks about his role at Laureate Institute for Brain Research is still accessible:
“I work part-time as a research psychiatrist for the assessment team at the Laureate Institute for Brain Research. We do research diagnostic assessments for a variety of imaging, genetic and biomarkers studies in mood, anxiety and other brain disorders. I also provide review and analysis of neuroscience research on my blog Brain Posts that can be found at www.brainposts.blogspot.com. You can follow me on Twitter @WRY999. I also use my blog and Twitter feed to share my bird photography images.”
I respected and admired Dr. Yates, as I’m sure many learners did. I will always remember Bill as a gifted scientist and teacher.
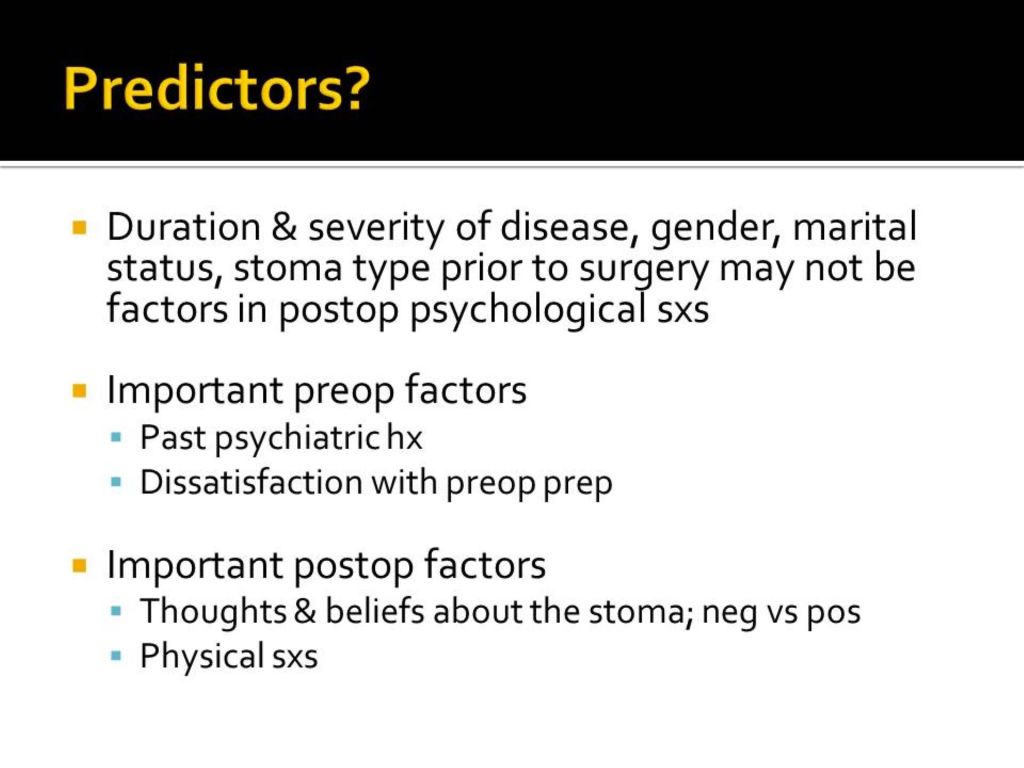
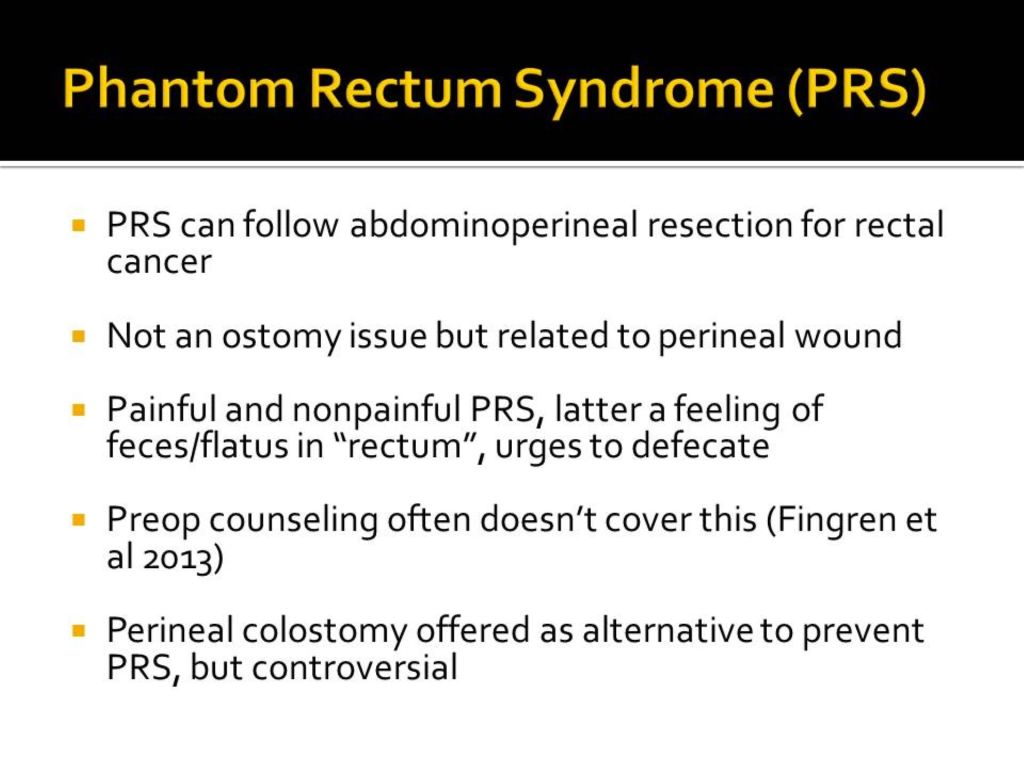
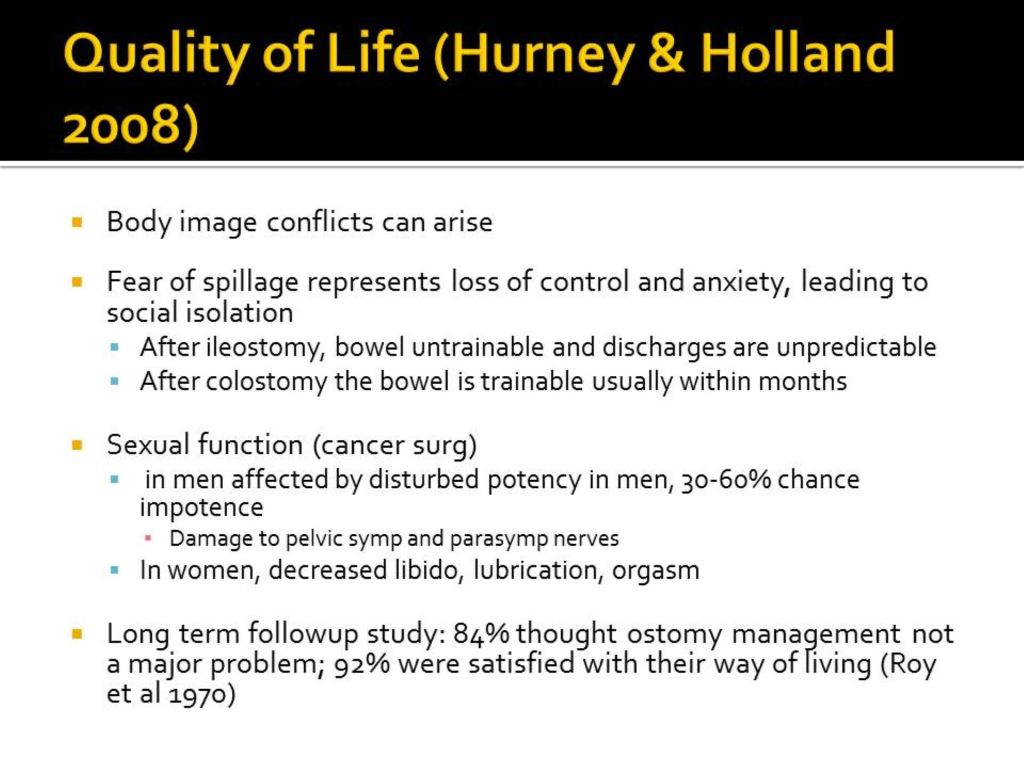
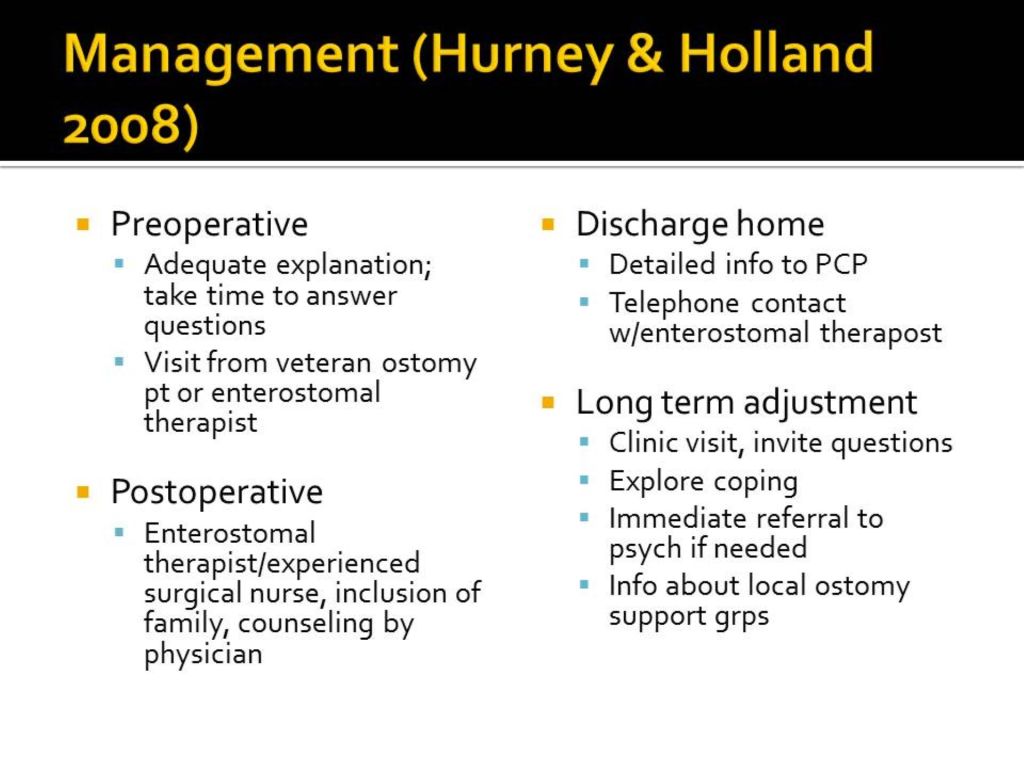
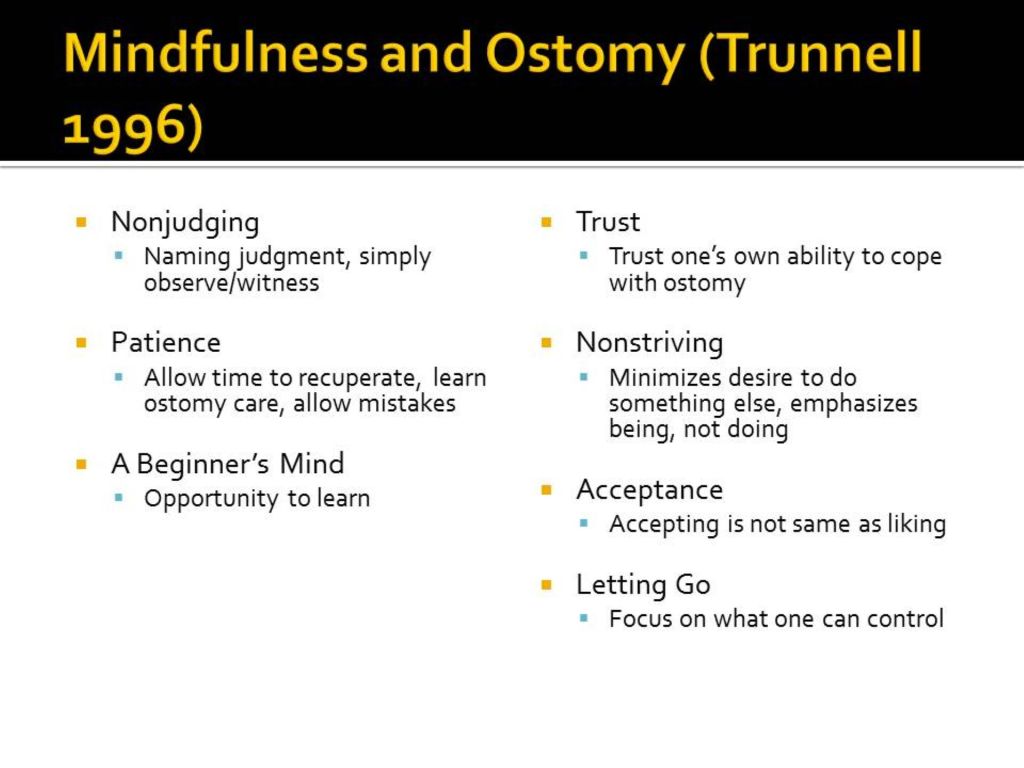
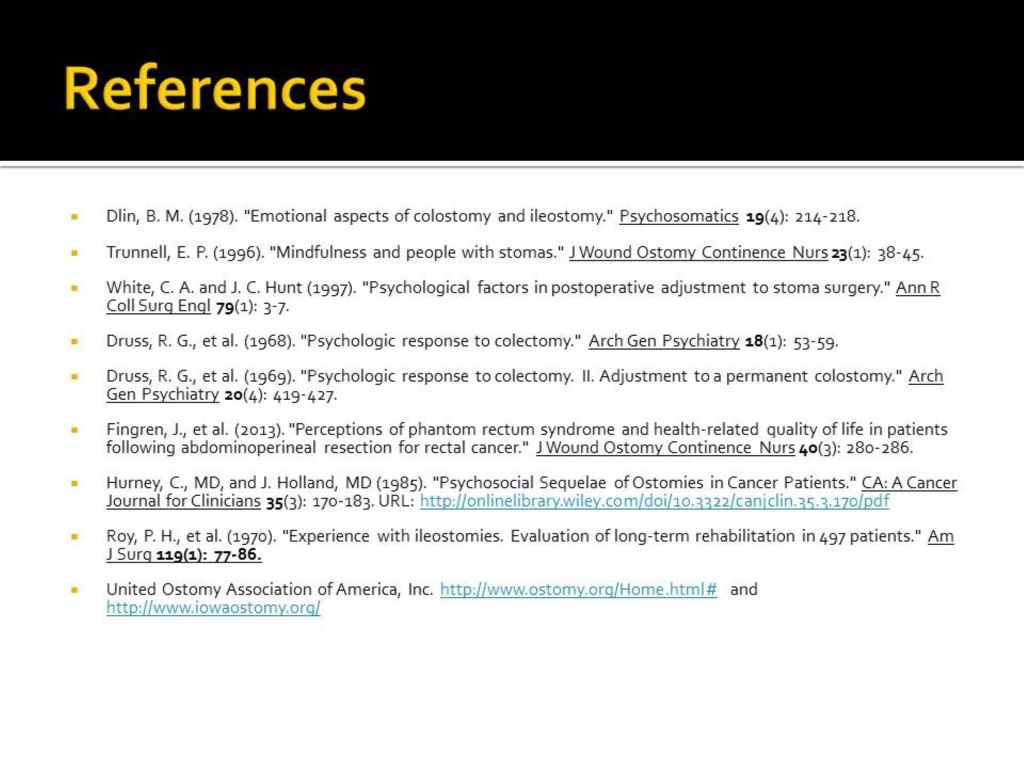
I think a fitting tribute would be to go ahead and post my CPCP on the psychosocial adjustment of patients with ostomy. One of the most interesting articles in the bibliography is how the mindfulness meditation approach to that adjustment can be very helpful. The website United Ostomy Association of America website is also informative.
The presentation is also limited to a dozen slides. I often encouraged learners to keep the number of slides to a managed number so the presentations wouldn’t run too long. I called my slide sets the Dirty Dozens.
Many thanks to Dr. William R. Yates and my condolences to his family.