I thought I’d re-post something from my previous blog, The Practical Psychosomaticist, which I cancelled several years ago. The title is “Face Time versus Facebook.” I sound really old in it although it appeared in 2011.
I’m a little more comfortable with the concept of social media nowadays and, despite how ignorant I was back then, I later got accounts in Facebook, Twitter, and LinkedIn. I got rid of them several years later, mainly because all I did was copy my blog posts on them.
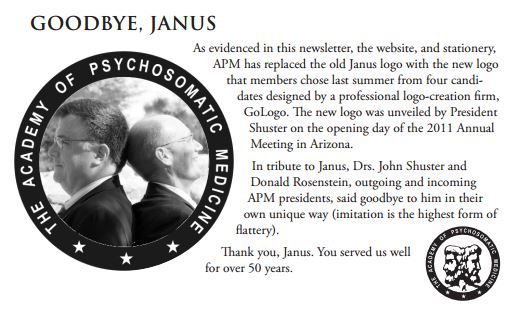
The Academy of Psychosomatic Medicine (APM) to which there is a link in the old post below, later changed its name to the Academy of Consultation-Liaison Psychiatry (ACLP), which made good sense. I still have the email message exchange in 2016 with Don R. Lipsitt, who wrote the book “Foundations of Consultation-Liaison Psychiatry: The Bumpy Road to Specialization.” It’s an excellent historical account of the process.

Don liked a post I wrote, entitled “The Time Has Come for ‘Ergasiology’ to Replace ‘Psychosomatic Medicine?” It was a humorous piece which mentioned how many different names had been considered in the past for alternative names for Psychosomatic Medicine. I was actually plugging his book. I don’t think ergasiology was ever considered; I made that part up. But it’s a thing. It was Adolph Meyer’s idea to invent the term from a combination of Greek words for “working” and “doing,” in order to illustrate psychobiology. Don thought “…the Board made a big mistake…” naming our organization Psychosomatic Medicine. He much preferred the term “consultation-liaison psychiatry.” We didn’t use emoticons in our messages.
The Don R. Lipsitt Award for Achievement in Integrated and Collaborative Care was created in 2014 to recognize individuals who demonstrate “excellence and innovation in the integration of mental health with other medical care…”
I don’t think the ACLP uses Facebook anymore, but they do have a Twitter account.
I also included in the old post a link to the Neuroleptic Malignant Information Service (NMSIS). I used to call the NMSIS service early in my career as a consultation-liaison psychiatrist. I often was able to get sound advice from Dr. Stanley Caroff.
Blog: Face Time versus Facebook
You know, I’m astounded by the electronic compensations we’ve made over the years for our increasingly busy schedules which often make it impossible to meet face to face. Frankly, I’ve not kept up. I still think of twittering as something birds do. If you don’t get that little joke, you’re probably not getting mail from the AARP.
The requests for psychiatric consultations are mediated over the electronic medical record and text paging. Technically the medical team that has primary responsibility for a patient’s medical care contacts me with a question about the psychiatric management issues. But it’s not unusual for consultation requests to be mediated by another consultant’s remarks in their note. The primary team simply passes the consultant’s opinion along in a request. They may not even be interested in my opinion.
I sometimes get emails from people who are right across the hall from me. I find it difficult to share the humor in a text message emoticon. And I get more out of face-to-face encounters with real people in the room when a difficult case comes my way and I need to tap into group wisdom to help a patient. These often involve cases of delirium, an acute confusional episode brought on by medical problems that often goes unrecognized or is misidentified as one of the many primary psychiatric issues it typically mimics.
The modern practice of medicine challenges practitioners and patients alike to integrate electronic communication methods into our care systems. And these methods can facilitate education in both directions. When professionals are separated geographically, whether by distances that span a single hospital complex or across continents, electronic communication can connect them.
But I can’t help thinking there are some messages we simply can’t convey with emoticons. By nature, humans communicate largely by nonverbal cues, especially in emotionally charged situations. And I can tell you, emotions get involved when physicians and nurses cue me that someone who has delirium is just another “psych patient” who needs to be transferred to a locked psychiatric unit (although such transfers are sometimes necessary for the patient’s safety).
So, when do we choose between Face Time and Facebook? Do we have to make that choice? Can we do both? When we as medical professionals are trying to resolve amongst ourselves what the next step should be in the assessment and treatment of a delirious patient who could die from an occult medical emergency, how should we communicate about that?
As a purely hypothetical example (though these types of cases do occur), say we suspect a patient has delirium which we think could be part of a rare and dangerous medical condition known as neuroleptic malignant syndrome (NMS). NMS is a complex neuropsychiatric disorder which can be marked by delirium, high fever, and severe muscular rigidity among other symptoms and signs. It can be caused very rarely by exposure to antipsychotic drugs such as Haloperidol or the newer atypical antipsychotics. The delirium can present with another uncommon psychiatric disorder called catatonia, and many experts consider NMS to be a drug-induced form of catatonia. Patients suffering from catatonia can display a variety of behaviors and physiologic abnormalities though they are often mute, immobile, and may display bizarre behaviors such as parroting what other people say to them, assuming very uncomfortable postures for extended periods of time (called waxy flexibility), and very rapid heart rate, sweating, and fever. The treatment of choice is electroconvulsive therapy (ECT) which can be life-saving.
Since NMS is rare, many consulting psychiatrists are often not confident about their ability to diagnose the condition. There may not be any colleagues in their hospital to turn to for advice. One option is to check the internet for a website devoted to educating clinicians about NMS, the Neuroleptic Malignant Syndrome Information Service at www.nmsis.org. The site is run by dedicated physicians who are ready to help clinicians diagnose and treat NMS. Physicians can reach them by telephone or email and there are educational materials on the website as well. I’ve used this service a couple of times and found it helpful. The next two electronic methods I have no experience with at all, but I find them intriguing.
One might be a social network like Facebook. In fact, the Academy of Psychosomatic Medicine (APM) has a Facebook link on their website, www.apm.org. Psychosomaticists can communicate with each other about issues broached at our annual conferences, but probably not discuss cases. Truth to tell, the Facebook site doesn’t look like it’s had many visitors. There are 3 posts which look like they’ve been there for a few months:
Message 1: We have been thinking about using Facebook as a way to continue discussions at the APM conference beyond the lectures themselves. Would anyone be interested in having discussions with the presenters from the APM conference in a forum such as this?
Message 2: This sounds great!
Message 3: I think it’s a very good idea
It’s not exactly scintillating.
Another service could be something called LinkedIn, which I gather is a social network designed for work-at-home professionals to stay connected with colleagues in the outside world. Maybe they should just get out more?
Email is probably the main way many professionals stay connected with each other across the country and around the world. The trouble is you have to wait for your colleague to check email. And there’s text messaging. I just have a little trouble purposely misspelling words to get enough of my message in the tiny text box. And I suppose one could tweet, whatever that is. You should probably just make sure your tweet is not the mating call for an ostrich. Those birds are heavy and can kick you into the middle of next week.
But there’s something about face time that demands the interpersonal communication skills, courtesy, and cooperation needed to solve problems that can’t be reduced to an emoticon.