The robins are building their Hurrah’s nests in our back yard again. That’s about the only thing that has not changed. The COVID-19 (C-19) pandemic has changed just about everything else in our lives.
I wear a face shield now at the hospital. We’re told to wear it as much as possible, like putting on our clothes in the morning. Don’t we leave them on all day? The shield keeps you from touching your face, which is why it’s better than a face mask. However, I’ve noticed something about wearing the face shield for much of the day. Before I describe it, let me give you analogy: If you’ve ever worked detasseling corn when you were young a long time ago, you might remember what happened when you closed your eyes at night and tried to go to sleep. I saw corn fields—miles and miles of corn fields. When I opened my eyes, the vision would disappear. But as soon as I closed my eyes again, I saw the vast corn fields.
It’s crazy, but I have a similar sensory after-effect when I doff my face shield–sometimes I still feel the headband. The pressure of it is just the same as if I were still wearing it. I suppose it’s because I cinch it too tightly. But if I don’t, it slips down my brow, pushing my eyeglasses down my nose.

Another change—I’m a Consultation-Liaison (C-L) Psychiatrist, so I’m used to washing my hands in between patients in the hospital. Now, I’ve got something I’ve never had before–alligator hide patterns on the backs of my hands. They’re dry and cracked. I don’t count the number of times I wash my hands, but it’s a lot more frequent than I used to do. It’s not uncommon for health care professionals to wash hands 75-100 times a day in the C-19 era. I have to use hand cream conscientiously—something I almost never did.
I’m less comfortable being closer than several feet away from people. I tend to hug the walls and corners in stairwells, where I now encounter more people than I ever have before. I guess the message everyone hears is “Stand by me—six feet away if you please.”
I don’t shake hands anymore. The lines into the hospital sometimes lead to crowding while we wait to have our temperatures taken and answer the screening questions about whether we’ve had fever, cough, shortness of breath, etc. It’s perfunctory most of the time, because virtually always the answer is “no” and everybody is in a hurry.
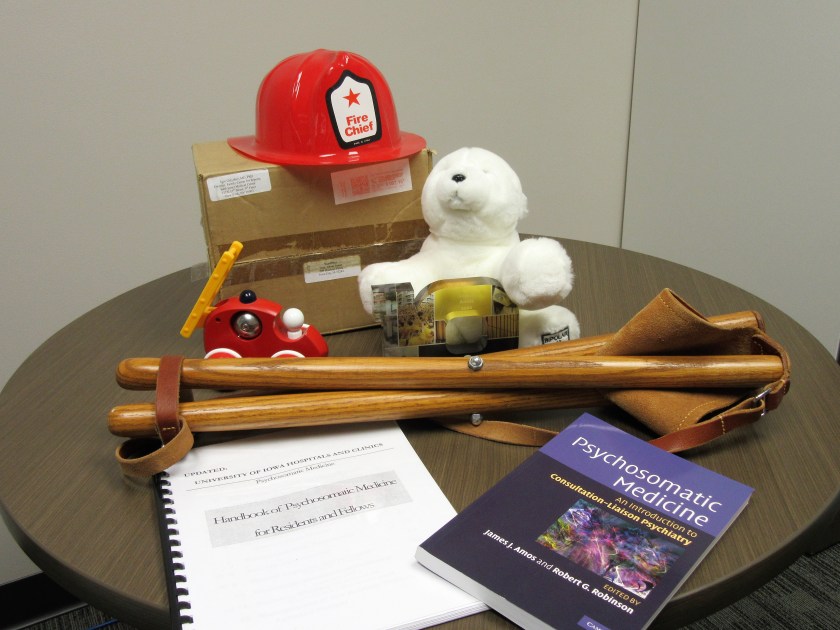
I don’t carry my little camp stool with me anymore, which allowed me to sit down with patients and have face to face, eye level interaction. I’m distinctly uncomfortable standing over them because I haven’t done that in years. If there is a chair in the room, I’m hesitant to use it because, like the camp stool, I worry that it might carry C-19 virus on its surface.

I used to evaluate psychiatric patients in our emergency room by simply going there and seeing them face to face, either in their rooms or, when it was really busy (which is most of the time), in the hallways.
I just used a remote telehealth interface platform using an iPad the other day, which allows me to interview patients from my office, in order to avoid the risk of contagion. It was a little slow and awkward, and I was uncomfortable that a health care professional had to be in the emergency room to hold it up for the patient—who was covered in blood. I felt a little guilty.
I used to round with medical students and residents on our patients. We were the movable feast, a sort of MASH (Mobile Army Surgical Hospital) unit, more like Mobile Unifying Shrink Hospital (MUSH). Unifying means unifying medicine and psychiatry. The medical students are not permitted on the wards now, in order to protect them. It’s awkward rounding with only one resident at a time, although another resident can do other things like chart review and telephone relatives for collateral history. I get in the hospital earlier nowadays, and see many non-C-19 patients alone without trainees, preparing for the C-19 surge when I expect we’ll get many more consultation requests to help care for C-19 patients with delirium and depression. It’s a one-man hit-and-run psychiatry consult service and efficiency is mandatory to meet the demand.
I see patients by myself for another reason. Try as we might, C-19 positive patients will slip through the screens. Many are asymptomatic but contagious, and any test will have false negative results. The idea is to expose the least number of health care front line staff members as possible. Faculty capacity is stretched pretty thin, which is pretty much the situation everywhere. I have to choose. I’m older. I’m weeks from retirement. I’m afraid.
But robins don’t have the burden of choice. They obey their instinct every spring, just the same.